Stroke: Difference between revisions
imported>Nancy Sculerati No edit summary |
imported>Nancy Sculerati |
||
| Line 22: | Line 22: | ||
===Temporary (or transient) ''strokes''=== | ===Temporary (or transient) ''strokes''=== | ||
A '''[[Transient Ischemic Attack]]''' (TIA) is a ''brief'' loss of neurologic function. In a TIA, the affected brain cells were not killed, but only transiently deprived of blood supply and the signs of what seems to be a stroke, (or black-out), pass quickly and ''completely''. TIA can certainly be a warning sign of an impending stroke, however, like a true stroke, is a | A '''[[Transient Ischemic Attack]]''' (TIA) is a ''brief'' loss of neurologic function. In a TIA, the affected brain cells were not killed, but only transiently deprived of blood supply and the signs of what seems to be a stroke, (or black-out), pass quickly and ''completely''. TIA can certainly be a warning sign of an impending stroke, however, and like a true stroke, is a neurologic emergency. None the less, a TIA is ''not'' a true stroke. | ||
===Broken blood vessel or blocked blood vessel?=== | |||
Strokes can be classified as '''ischemic''' or '''hemorrhagic'''. | |||
===Ischemic strokes=== | ===Ischemic strokes=== | ||
The word ischemia indicates the loss of blood supply to tissues. When tissues are ischemic, they are generally pale and, if the ischemia persists long enough, become swollen and change further as cells swell and then die. The area of dead (also called necrotic) tissue that results from ischemia is called an [[Infarct|infarct]]. | The word ischemia indicates the loss of blood supply to tissues. When tissues are ischemic, they are generally pale and, if the ischemia persists long enough, become swollen and change further as cells swell and then die. The area of dead (also called necrotic) tissue that results from ischemia is called an [[Infarct|infarct]]. | ||
Revision as of 09:45, 2 May 2007
A stroke (syn. Cerebral Vascular Accident or "CVA") is a sudden, often focal, loss of brain function. That term "cerebral vascular accident" summarizes the underlying cause and nature of a stroke: (1) "cerebral" indicates that the brain is involved (2) "vascular" indicates that blood vessels are involved and (3) "accident" indicates that this is a rapid and detrimental event. Although most strokes in people do involve the higher centers of the brain that are located in the cerebral hemispheres; the word cerebral is not strictly accurate, as some strokes can involve only the lower portions of the brain, like the medulla oblongata or other areas of the brain stem. Most stroke experts prefer the term "stroke" to "CVA", but both are used commonly to refer to this acquired neurological disorder.
There are many different causes of stroke, but whenever a stroke occurs, there has been an interruption of the normal bood supply to brain cells. When that interruption is long enough, it causes death of brain cells. The symptoms and signs of disease that are caused by the death of brain stems is highly dependant upon the number of cells that are affected, and exactly where these affected cells are located in the brain. Accordingly, strokes can have many different clinical presentations - ranging from deep coma with the loss of the ability to breathe; to very limited deficits in the ability to move a part of the body, or changes in sensory perception like partial blindness from a restriction in visual field, without any associated problems with movement.
The interuption of normal blood circulation to the brain, or to limited and specific areas of the brain, generally comes about either because blood flow is stopped (occluded) within the blood vessel, or because the blood vessel ruptures (hemorrhages) and no longer serves to supply the brain cells with nutrients and oxygen. Hemmorhages hurt the brain in ways besides starving cells, the break in the vessels from a hemmorhage floods the blood it carries into an expanding clot that puts damaging pressure on these cells, as well as depriving them of vital supplies.
Ordinarily, at least some brain tissue is injured by a stroke - yet not killed. The injury to these cells is reversible. That's one reason why the amount of recovery during the initial time period after a stroke is difficult to predict, and also why treatment at that time can influence the course of recovery. If the stroke patient survives the stroke, some brain cells may actually recover in time if the injury was not too great. Since the central nervous system, even in older adults, has at least some ability to adjust to loss (Plasticity), such that other areas of the brain can often take over partial functions of the damaged areas, there may be more recovery of function over time for the patient, even once the damaged areas of the brain are no longer capable of any additional recovery of injured brain cells.
For survivors of stroke, treatment is important at least three time periods after the incident. Immediate treatment in the minutes and hours after the first signs of a stroke can sometimes change the course of the acute event by removing factors (like an embolus or extreme hypertension) that will otherwise promotegreater and greater injury. Treatment after the acute stroke rehabilitation therapy can offer the best hope of maximal recovery for most patients by aiding the person's ability to use their surviving brain to take over some of the functions that damaged tissues cannot manage, and long term therapy can help reduce the underlying risks of another stroke.
Epidemiology
Stroke is one of the leading causes of long term disabilty, and of death, in the developed world. Approximately 700,000 Americans per year experience a stroke. It is the third leading cause of death and the leading cause of long-term adult disability in the United States.[1] On average, a stroke occurs every 45 seconds and someone dies from a stroke every 3 minutes.[2][3]
Risk factors for stroke include atherosclerosis, advanced age, hypertension (high blood pressure), diabetes mellitus, high cholesterol, cigarette smoking, atrial fibrillation, ethnic identity, and some blood clotting disorders.
The term "brain attack" has been advocated for use in the United States for stroke, just as the term "heart attack" is used for myocardial infarction. Many hospitals have multidisciplinary "stroke teams" specifically for swift treatment of stroke.
Types of Stroke
This section aims to lay out the types of strokes so that the rest of the article is more easily understood. Strokes can be classified according to the mechanism of injury, and also according to the areas of the brain that are injured.
Temporary (or transient) strokes
A Transient Ischemic Attack (TIA) is a brief loss of neurologic function. In a TIA, the affected brain cells were not killed, but only transiently deprived of blood supply and the signs of what seems to be a stroke, (or black-out), pass quickly and completely. TIA can certainly be a warning sign of an impending stroke, however, and like a true stroke, is a neurologic emergency. None the less, a TIA is not a true stroke.
Broken blood vessel or blocked blood vessel?
Strokes can be classified as ischemic or hemorrhagic.
Ischemic strokes
The word ischemia indicates the loss of blood supply to tissues. When tissues are ischemic, they are generally pale and, if the ischemia persists long enough, become swollen and change further as cells swell and then die. The area of dead (also called necrotic) tissue that results from ischemia is called an infarct.
- Ischemic strokes make up about 87% of all strokes and can be due to blockage of a feeding artery by a clot or by generalized low blood flow (hypoperfusion), along with narrowed arteries. Lacunae, or small vessel ischemic strokes, are responsible for about 20% of all strokes and are common in hypertension and diabetes mellitus.
- Hemorrhagic strokes are usually classed as either intracerebral hemorrhage or subarachnoid hemorrhage.[4] Uncontrolled hypertension is a leading cause of hemorrhagic stroke. Weaknesses in brain arteries, (for example, aneurysms) can cause hemorrhagic strokes even when the pressure of the blood inside the arteries is not excessive. Because the brain is enclosed within a rigid structure (the skull), even a small amount of bleeding can cause a dramatic increase in pressure on the brain. This can lead to herniation, in which part of the brain is compressed through the base of the skull, causing rapid coma and death.
Etiology
The brain is made out of nerve cells and supporting cells, it is covered by protective layers and it is moistened by the constant circulation of a pristine fluid called "cerebrospinal fluid" (which is often abbreviated as CSF).
Like all parts of the body, the brain has vessels that pump blood to it from the heart called arteries and vessels that collect the blood after circulating through the organ for return to the heart called veins. As in most organs of the body, the arteries to the brain carry blood loaded with oxygen and glucose (blood sugar) and the veins carry away blood that has delivered these vital supplies to the cells of the brain and had their waste products dumped in it.
The blood circulation to the brain is ordinary in these ways, but since brain cells are more vulnerable to loss of oxygen and glucose than are the cells of any other portion of the body, there are special features of the vasculature to the brain that are protective. One of these extra-ordinary features is the architectural design of the blood delivery system to the brain. It is a circle of arteries that joins blood pumped up from the front of the neck ( the carotid arteries) from blood pumped up from the back (the vertebral arteries). In most healthy young people, this system of blood flow is so good that even if one of the arteries is lost altogether (from an injury, for example), the others can make up for it and keep delivering a properly working circulation of fresh arterial blood, and no impairment to the brain cells occurs.
Ischemic Stroke
Atherosclerosis is responsible for the majority of ischemic strokes. Atheroembolism can occur within the cerebral circulation or can originate outside the cerebral circulation. The etiology of atherosclerosis-related strokes is very similar to that of heart attacks. An atherosclerotic plaque in a cerebral artery can gradually develop an associated thrombus or rupture suddenly causing a rapid occlusion, or the thrombus can break off and lodge in a vessel even deeper in the brain. "Thrombotic stroke" usually refers to in-situ thrombus, "embolic stroke" to thrombi that travel from distant sites.
Thrombotic Stroke
Thrombotic and thromboembolic strokes can originate in either large or small blood vessels, and are usually due to abnormalities in the vessel (most commonly atherosclerosis). One of the most important etiologies is carotid artery disease. Lacunae are also a subset of thrombotic stroke.
Embolic Stroke
Embolism of thrombi from outside the cerebral circulation are responsible for a large and important subset of ischemic strokes. In these cases a thrombus (blood clot) travels from its origin and lodges in a cerebral artery. Most of these strokes are of cardiac origin (Cardioembolic).
Cardioembolic Stroke
- Atrial fibrillation: The majority of embolic strokes originating in the heart are due to atrial fibrillation. In fact, about 16% of strokes are associated with atrial fibrillation, and the presence of atrial fibrillation increases stroke risk by about 5-11% per year, depending on other risk factors. [5]The relative stasis of blood in the left atrium leads to blood clot formation, and these clots can be expelled from the heart to enter the cerebral circulation.
- Mural thrombi: anything that causes blood flow in the heart to slow can cause thrombus formation. This includes thrombi formed in the atrial appendage and thrombi formed in the left ventricle in patients with heart failure.
- Valvular heart disease: this includes rheumatic heart disease, infective endocarditis, and presence of a prosthetic heart valve.
- Paradoxical embolism: this occurs primarily when a deep venous thrombosis (DVT) in the leg breaks off, passing through a patent foramen ovale (PFO) into the left ventricle, and then to the brain.
Systemic hypoperfusion (Watershed stroke)
Systemic hypoperfusion is the reduction of blood flow to all parts of the body. It is most commonly due to various types of shock. Hypoxemia (low blood oxygen content) may precipitate the hypoperfusion. Because the reduction in blood flow is global, all parts of the brain may be affected, especially "watershed" areas --- border zone regions supplied by the major cerebral arteries. Blood flow to these areas does not necessarily stop, but instead it may lessen to the point where brain damage can occur.
Hemorrhagic stroke
A hemorrhagic stroke, or cerebral hemorrhage, is a form of stroke that occurs when a blood vessel in the brain ruptures or bleeds. There are two types of hemorrhagic stroke: intracerebral hemorrhage, and subarachnoid hemorrhage (SAH). Traumatic hemorrhage, including epidural hemorrhage, subdural hemorrhage, and some SAH are usually considered separately.
Intracerebral hemorrhage
Intracerebral hemorrhage (ICH) is bleeding directly into the brain tissue, forming a gradually enlarging hematoma (pool of blood). It generally occurs in small arteries or arterioles and is commonly due to hypertension, trauma, and vascular malformations. The hematoma enlarges until pressure from surrounding tissue limits its growth, or until it decompresses by emptying into the ventricular system. ICH has a mortality rate of 44 percent after 30 days, higher than ischemic stroke or even the very deadly subarachnoid hemorrhage.[6]
Subarachnoid hemorrhage
Subarachnoid hemorrhage (SAH) is bleeding into the cerebrospinal fluid (CSF) surrounding the brain. The two most common causes of SAH are rupture of aneurysms and bleeding from vascular malformations. Bleeding into the CSF from a ruptured aneurysm occurs very quickly, causing rapidly increased intracranial pressure. The initial bleed can be brief, but rebleeding is common. Death or deep coma ensues if the bleeding continues. SAH has a 37-45% mortality for patients 45 and older.[7][8]Cerebral aneurysms can be associated with other disorders, such as adult polycystic kidney disease.
Risk Factors
Many factors are generally agreed to cause a higher risk for a stroke.[9]
- Previous stroke
- Atherosclerosis: many of the risk factors listed below are also risk factors for atherosclerosis. Other marker for atherosclerosis include peripheral artery disease and coronary artery disease.
- Hypertension is the most powerful risk factor for ischemic stroke, and the primary risk factor for intracerebral hemorrhagic stroke. [10][11]
- Smoking: cigarette smoking significantly increases stroke risk, and the risk is dependent on the amount of smoking.[12] Cigar and pipe smoke also increase stroke risk but to a lesser degree.
- Transient Ischemic Attack: Occurrence of TIA is a strong risk factor for stroke. In one study, 5% of patients with TIA developed stroke within 2 days, 10% within 90 days.[13] TIA should be considered a medical emergency; rapid response reduces the risk of stroke.
- Atrial Fibrillation (AF): The average yearly risk for stroke in untreated AF is 5%, but can be as high as 12%.[14]
- Diabetes mellitus: Diabetes is a major stroke risk.[15]
- Age: the risk of stroke in adults increases significantly over the age of 55, and continues to increase thereafter.
- Ethnicity: African Americans have twice the risk of a first stroke as whites.
- Carotid stenosis (asymptomatic)
- Cocaine: cocaine use is a significant risk for stroke and heart attack.
- Blood disorders (e.g. sickle-cell disease, anti-cardiolipin syndrome)
- Estrogen: recent studies have found small but significant increase in stroke risk in women receiving hormone replacement therapy (HRT). In one large study, stroke risk was increase by 55%, which equates to 12 additional strokes per 10,000 person-years.[16] Oral contraceptive pills (OCPs) may confer some risk, especially when combined with other risks such as smoking, however the risk from the currently used low-dose OCPs is quite low.[17]
- Pregnancy: there is a small but significant increase in stroke risk during, and just after pregnancy.
Symptoms
The symptoms of stroke depend on what part of the brain is affected. A friend or family member may be the first to notice. Symptoms can include:
- Sudden numbness or weakness of the face, arm, or leg, especially one-sided
- Sudden confusion, trouble speaking, or trouble understanding
- Sudden trouble walking, dizziness, or loss of balance or coordination
- Sudden trouble seeing in 1 or both eyes
- Sudden severe headache
- Difficulty swallowing or drooling
Diagnosis
A stroke is diagnosed first by a medical professional taking a proper history and physical exam. Addtional tests include:
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI)
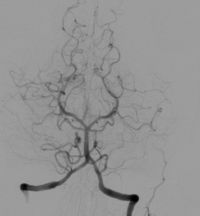
- Cerebral angiography
Treatment
Stroke is a medical emergency. Permanent neurologic damage or death can sometimes be avoided, but only if stroke is promptly diagnosed and treated.
Thrombolysis
Presentation to a specialized stroke center within 3 hours of the start of symptoms may allow for the reversal of the stroke by adminstration by clot-disolving medications, or thrombolytics. Tissue Plasminogen Activator (tPA) is the usual agent. Studies have shown that tPA given within 6 hours of the onset of stroke symptoms significantly reduces death and dependency, but there is a significant risk of bleeding, especially intracranial hemorrhage. If given within 3 hours, outcomes are improved, and risk is reduced.[18][19]
Prevention
Prevention of stroke involves reducing modifiable risk factors, and falls broadly into two categories: prevention of first stroke (primary prevention), and prevention of further strokes (secondary prevention). Also, some risk factors are modifiable (e.g. smoking), and some are not (e.g. age). Prevention, especially secondary prevention, involves certain medications.
Risk factor reduction
- Keeping blood pressure below 120/80 reduces the risk of both primary and recurrent stroke.[10][11]
- Quitting smoking decreases risk significantly 2 years after quitting cigarettes.[12]
- Transient ischemic attack (TIA) is a brief period of stroke symptoms, and is a warning sign of impending stroke. Seeking emergency medical attention reduces the risk of stroke after TIA.
- The risk of stroke due to atrial fibrillation can be significantly reduced with the use of oral anticoagulants (i.e. warfarin).[20][21]
- Diabetes is a major stroke risk factor. The role of good blood sugar control in the prevention of stroke in diabetics is still being investigated. Aggressive treatment of cholesterol and blood pressure in diabetics is essential. Certain medications help prevent strokes in diabetics.[22][23]
- High Cholesterol: treatment of high cholesterol and other blood lipid disorders reduces the rate of first stroke and recurrent stroke. [24]
Medications
- Aspirin
- Plavix
- Aggrenox
- Warfarin
- HMG-CoA reductase inhibitors (Statins)
- Angiogensin converting enzyme (ACE) inhibitors
References
- ↑ Centers for Disease Control and Prevention (CDC). Prevalence of disabilities and associated health conditions among adults: United States, 1999. MMWR Morb Mortal Wkly Rep. 2001; 50: 120–125
- ↑ Circulation. 2007;115:e69-e171.
- ↑ http://circ.ahajournals.org/cgi/content/full/CIRCULATIONAHA.106.179918
- ↑ Goldman: Cecil Textbook of Medicine, 22nd ed., Copyright © 2004 W. B. Saunders Company
- ↑ Robert G. Hart, MD Jonathan L. Halperin, MD. Atrial Fibrillation and Stroke Concepts and Controversies. Stroke. 2001;32:803.
- ↑ Caplan LR (1992). "Intracerebral hemorrhage". Lancet 339 (8794): 656-8. PMID 1347346.
- ↑ El-Saed A, Kuller LH, Newman AB, Lopez O, Costantino J, McTigue K, Cushman M, Kronmal R. Geographic variations in stroke incidence and mortality among older populations in four US communities. Stroke. 2006; 37: 1975–1979.
- ↑ Rosamond WD, Folsom AR, Chambless LE, Wang CH, McGovern PG, Howard G, Copper LS, Shahar E. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerotic Risk in Communities (ARIC) Cohort. Stroke. 1999; 30: 736–743
- ↑ Goldstein LB. Adams R. Alberts MJ. Appel LJ. Brass LM. Bushnell CD. Culebras A. DeGraba TJ. Gorelick PB. Guyton JR. Hart RG. Howard G. Kelly-Hayes M. Nixon JV. Sacco RL. American Heart Association. American Stroke Association Stroke Council. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 113(24):e873-923, 2006 Jun 20
- ↑ 10.0 10.1 ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial.Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT).JAMA. 288(23):2981-97, 2002 Dec 18.
- ↑ 11.0 11.1 Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Au R, Kannel WB, Wolf PA. The lifetime risk of stroke: Estimates from the Framingham study. Stroke. 2006; 37: 345–350
- ↑ 12.0 12.1 Wolf PA, D’Agostino RB, Kannel WB, Bonita R, Belanger AJ. Cigarette smoking as a risk factor for stroke: the Framingham study. JAMA. 1988; 259: 1025–1029
- ↑ Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA. 2000; 284: 2901–2906
- ↑ Hylek E. M., Go A. S., Chang Y., Jensvold N. G., Henault L. E., Selby J. V., Singer D. E. N Engl J Med 2003; 349:1019-1026, Sep 11, 2003
- ↑ Stroke in Patients With Diabetes and Hypertension. Samy I. McFarlane, MD, MPH, Domenic A. Sica, MD, James R. Sowers, MD. J Clin Hypertens (Greenwich). 2005;7(5):286-292.
- ↑ Hendrix SL, Wassertheil-Smoller S, Johnson KC, Howard BV, Kooperberg C, Rossouw JE, Trevisan M, Aragaki A, Baird AE, Bray PF, Buring JE, Criqui MH, Herrington D, Lynch JK, Rapp SR, Torner J, WHI investigators. Effects of conjugated equine estrogen on stroke in the Women’s Health Initiative. Circulation. 2006; 113: 2425–2434
- ↑ Sasitorn Siritho, MD; Amanda G. Thrift, PhD; John J. McNeil, PhD; Roger X. You, PhD; Stephen M. Davis, MD Geoffrey A. Donnan, MD. Risk of Ischemic Stroke Among Users of the Oral Contraceptive Pill. The Melbourne Risk Factor Study (MERFS) Group. Stroke, Vol 22, 312-318
- ↑ Gregory W. Albers, MD; Wayne M. Clark, MD; Kenneth P. Madden, MD, PhD Scott A. Hamilton, PhD.ATLANTIS Trial:Results for Patients Treated Within 3 Hours of Stroke Onset 2002;33:493
- ↑ Joanna Wardlaw, Eivind Berge, Gergory delZoppo and Takenori Yamaguchi. Thrombolysis for acute ischemic stroke. Stroke. 2004;35:2914-2915.
- ↑ Stroke Prevention in Atrial Fibrillation Investigators. Stroke prevention in atrial fibrillation study: Final results. Circulation 1991; 84:527. Aspirin alone only minimally reduces stroke risk.
- ↑ Petersen, P, Boysen, G, Godtfredsen, J, et al. Placebo-controlled, randomized trial of warfarin and aspirin for prevention of thromboembolic complications in chronic atrial fibrillation. The Copenhagen AFASAK Study. Lancet 1989; 1:175.
- ↑ Timothy M. E. Davis, FRACP; Helen Millns, PhD; Irene M. Stratton, MSc; Rury R. Holman, FRCP; Robert C. Turner, MD, FRCP; for the UK Prospective Diabetes Study Group. Risk Factors for Stroke in Type 2 Diabetes Mellitus, United Kingdom Prospective Diabetes Study (UKPDS) 29.Arch Intern Med. 1999;159:1097-1103.
- ↑ PA Wolf, RB D'Agostino, AJ Belanger and WB Kannel Probability of stroke: a risk profile from the Framingham Study. Stroke, Vol 22, 312-318
- ↑ Blauw GJ, Lagaay AM, Smelt AH, Westendorp RG. (1997) Stroke, statins, and cholesterol. A meta-analysis of randomized, placebo-controlled, double-blind trials with HMG-CoA reductase inhibitors. Stroke May;28(5):946-50. PMID 9158630
External Links
- http://circ.ahajournals.org/cgi/content/full/CIRCULATIONAHA.106.179918
- http://www.cdc.gov/stroke/
- http://www.strokeassociation.org/presenter.jhtml?identifier=1200037
- http://www.nlm.nih.gov/medlineplus/ency/article/000726.htm